What Is a Gender Identity Clinic? A Complete Guide for Patients and Families
Understanding Gender Identity
Before discussing gender identity clinics, it helps to understand the term gender identity.
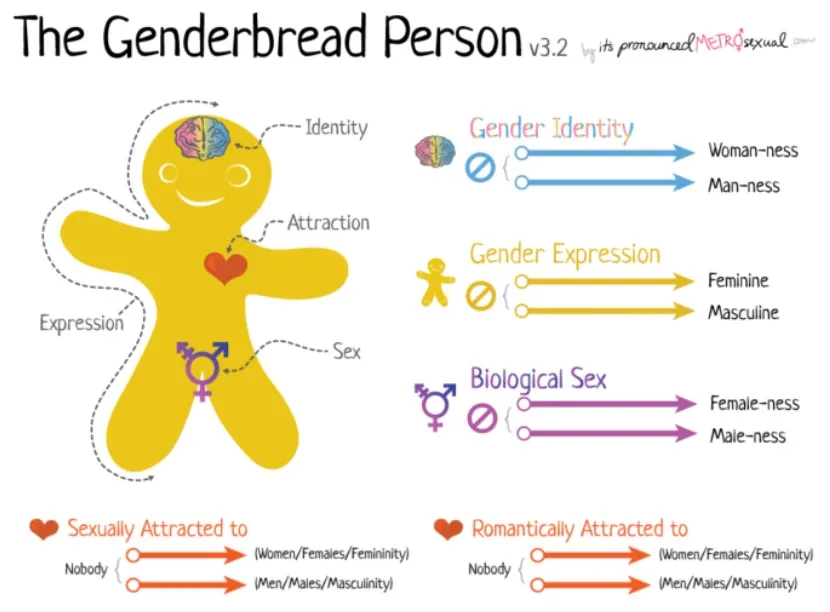
Gender identity refers to a person’s internal sense of their gender, which may be male, female, both, neither, or somewhere along a spectrum. This identity may or may not match the sex assigned at birth.
Some commonly used terms include:
-
Cisgender — when gender identity aligns with sex assigned at birth
-
Transgender — when gender identity differs from sex assigned at birth
-
Non-binary — gender identity outside the traditional male/female categories
-
Gender diverse — an umbrella term for varied gender identities
Gender identity is a personal and deeply individual experience, and healthcare providers aim to support patients respectfully and safely.
What Is a Gender Identity Clinic?
A gender identity clinic is a healthcare service that provides specialized medical, psychological, and social support for individuals exploring or affirming their gender identity.
These clinics typically operate within hospitals, community health centres, or specialized healthcare programs. Their goal is to provide evidence-based, compassionate, and coordinated care.
Gender identity clinics do not exist only for medical transition. They support people at many stages of their journey, including those who are still exploring their identity.
Who Gender Identity Clinics Help
Gender identity clinics serve a wide range of patients, including:
-
Children and adolescents questioning their gender identity
-
Adults seeking gender-affirming care
-
Transgender and non-binary individuals
-
Families looking for guidance and support
-
Patients seeking mental health counseling related to gender identity
Some patients visit once for information, while others receive ongoing care.
Services Offered at Gender Identity Clinics
Services vary depending on the clinic, but most gender identity clinics offer a multidisciplinary approach to care.
Assessment and Counseling
Mental health professionals often help patients:
-
Explore gender identity
-
Manage gender dysphoria
-
Navigate social transitions
-
Address anxiety or depression
-
Support family understanding
Counseling is not about changing identity, but about supporting well-being and informed decisions.
Hormone Therapy (Gender-Affirming Hormones)
Some clinics provide or coordinate hormone replacement therapy (HRT), such as:
-
Estrogen therapy
-
Testosterone therapy
-
Puberty blockers for youth (when appropriate)
These treatments are carefully monitored by healthcare professionals to ensure safety.
In Ontario, hormone therapy may sometimes be managed by trained family physicians or nurse practitioners, in collaboration with specialists.
Referrals for Gender-Affirming Surgery
Gender identity clinics often help patients access surgical services by providing:
-
Assessments
-
Documentation
-
Referrals to surgeons
-
Pre- and post-operative support
Examples of gender-affirming surgeries include:
-
Chest surgery
-
Breast augmentation
-
Gender-affirming genital surgery
-
Facial procedures
Not all patients choose surgery, and it is never required for gender identity validation.
Primary Care Coordination
Gender identity clinics frequently work alongside family doctors, who remain central to a patient’s overall healthcare.
A family physician may help with:
-
Routine checkups
-
Prescriptions
-
Preventive care
-
Lab monitoring
-
Referrals
At clinics like Halton Medix Milton, providers often help patients connect with appropriate specialized services when needed.
The Role of Family Doctors in Gender-Affirming Care
Family doctors are often the first point of contact for patients seeking gender identity care.
They may:
-
Discuss concerns about gender identity
-
Provide initial assessments
-
Refer patients to gender identity clinics
-
Prescribe hormone therapy (in some cases)
-
Coordinate mental health support
In Ontario’s healthcare system, family physicians play an important role in ensuring care remains accessible, continuous, and patient-focused.
Gender Identity Clinics in Ontario
Ontario has several gender identity programs, often located in larger healthcare centres. Wait times can vary depending on demand and location.
Examples of services available in Ontario include:
-
Hospital-based gender clinics
-
Community health centre programs
-
Youth gender identity services
-
Virtual consultation programs
Because demand has increased, many patients begin by speaking with a family doctor to explore options and referrals.
Is a Referral Required?
In many cases, yes — a referral from a family doctor or nurse practitioner is required to access a gender identity clinic.
This referral helps ensure patients are connected to the right services for their needs.
If you do not currently have a family doctor, a walk-in clinic or primary care clinic may help initiate the process.
Supporting Youth and Adolescents
Gender identity clinics often provide specialized care for children and teenagers.
Youth services may include:
-
Family counseling
-
Mental health support
-
Puberty blockers when medically appropriate
-
Education for parents and caregivers
Care for young patients focuses on well-being, safety, and informed decision-making.
Family involvement is often encouraged, but care remains patient-centered and respectful.
Mental Health and Gender Identity
Not everyone exploring gender identity experiences mental health challenges. However, supportive mental healthcare can be important for individuals dealing with:
-
Gender dysphoria
-
Social stress
-
Family conflict
-
Anxiety or depression
Gender identity clinics often include psychologists, social workers, or psychiatrists as part of the care team.
The goal is to support overall health — not just physical transition-related care.
Gender-Affirming Care Is Individualized
There is no single path for gender identity care.
Some patients may:
-
Seek counseling only
-
Use hormone therapy
-
Pursue surgery
-
Choose social transition without medical treatment
-
Decide not to pursue medical interventions
Gender identity clinics help patients make informed decisions at their own pace.
Accessing Care in Milton and Halton Region
Patients in Milton and the Halton region typically begin by speaking with a primary care provider.
A clinic like Halton Medix Milton can help by:
-
Providing a safe and respectful environment
-
Discussing patient concerns
-
Offering referrals to gender identity clinics
-
Coordinating ongoing care
Primary care providers help ensure patients do not feel alone navigating the healthcare system.
Common Questions About Gender Identity Clinics
Are gender identity clinics only for transgender patients?
No. These clinics support anyone exploring gender identity or seeking gender-affirming healthcare.
Do you need to be certain about your gender identity?
No. Many patients visit simply to learn, ask questions, or explore options.
Is gender-affirming care covered in Ontario?
Some services are covered by OHIP, including certain assessments and surgeries. Coverage depends on the treatment and eligibility criteria.
Can adults access care later in life?
Yes. Gender identity care is available for patients of all ages.
The Importance of Respectful Healthcare
Healthcare works best when patients feel:
-
Safe
-
Heard
-
Respected
-
Supported
Gender identity clinics aim to create inclusive environments where patients can receive evidence-based medical care without judgment.
Primary care clinics that collaborate with these services help ensure patients receive continuous and coordinated healthcare.
Final Thoughts
Gender identity clinics play an important role in modern healthcare by providing specialized support for gender-diverse individuals. They offer counseling, medical care, referrals, and long-term guidance tailored to each patient’s needs.
For many people in Ontario, the journey begins with a conversation with a family doctor or primary care provider. Clinics like Halton Medix Milton help patients access appropriate services while continuing to provide everyday healthcare.
Understanding what gender identity clinics do can make the process feel less overwhelming and help patients take the next step toward care with confidence.

